Osteoporosis is a widespread skeletal disorder that weakens bones, making them fragile and prone to fractures. Affecting over 200 million people globally, it poses a major public health challenge. The disease develops when bone resorption outpaces bone formation, leading to reduced bone density and structural deterioration.
This “silent disease” progresses without symptoms until a sudden fracture occurs—often in the spine, hip, or wrist. Vertebral fractures can cause chronic pain, height loss, and even breathing difficulties due to spinal deformities. Hip fractures are particularly dangerous, linked to high mortality rates and significant healthcare costs.
While bone loss naturally accelerates with age—especially in postmenopausal women due to estrogen decline—early detection and proper management can help prevent severe complications. Understanding risk factors, maintaining bone health through nutrition and exercise, and timely medical intervention are key to reducing osteoporosis’s impact.
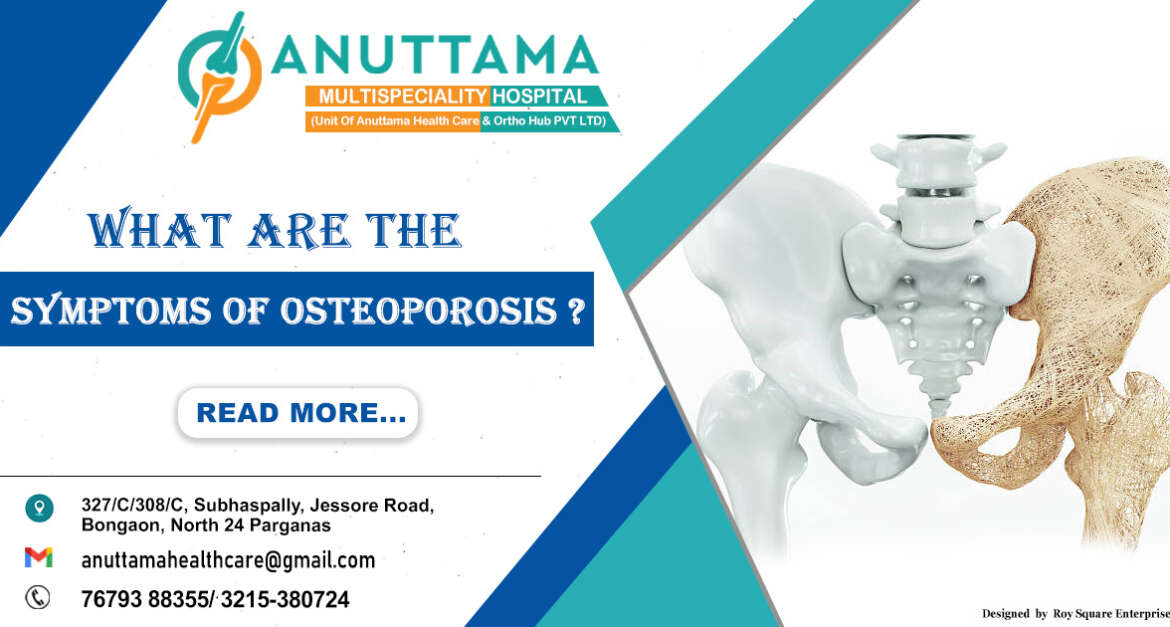
What Are the Symptoms of Osteoporosis?
Osteoporosis typically progresses silently until complications arise. The most common clinical manifestations include:
1. Fragility Fractures:
– Occur from minimal trauma (fall from standing height or less)
– Most frequent sites: vertebral bodies (especially T12-L2), femoral neck, distal radius
– Vertebral fractures may present as acute back pain or be discovered incidentally on imaging
– Hip fractures often require surgical intervention and carry high morbidity/mortality
2. Height Loss and Postural Changes:
– Progressive loss of height (>1.5 inches) suggests vertebral compression fractures
– Development of thoracic kyphosis (dowager’s hump) from multiple vertebral fractures
– Protuberant abdomen due to reduced space between rib cage and pelvis
3. Chronic Pain:
– Persistent back pain from vertebral fractures
– Muscle fatigue and spasm from altered biomechanics
– Secondary osteoarthritis from abnormal joint loading
4. Functional Impairments:
– Reduced mobility and balance issues increasing fall risk
– Trouble doing everyday tasks
– Respiratory compromise from severe kyphosis
It’s crucial to recognize that many vertebral fractures are asymptomatic initially, with only about one-third coming to clinical attention. This underscores the importance of proactive screening in high-risk populations rather than waiting for symptoms to develop.
What Causes Osteoporosis?
The etiology of osteoporosis is multifactorial, involving an interplay between genetic predisposition and environmental influences:

1. Hormonal Factors
– Estrogen Deficiency: Postmenopausal state is the most common cause, with rapid bone loss in the first 5-7 years after menopause
– Hypogonadism in Men: Low testosterone reduces osteoblastic activity
– Hyperparathyroidism: PTH excess increases bone resorption
– Hyperthyroidism: Both endogenous and iatrogenic (excessive thyroid hormone replacement)
– Cushing’s Syndrome: Glucocorticoid excess inhibits osteoblast function
2. Nutritional Deficiencies
– Calcium: Chronic inadequate intake (<500 mg/day) leads to secondary hyperparathyroidism
– Vitamin D: Deficiency (<20 ng/mL) impairs calcium absorption and bone mineralization
– Protein: Inadequate protein (<0.8 g/kg/day) compromises bone matrix formation
– Other Micronutrients: Magnesium, vitamin K, zinc, and copper all play important roles
3. Secondary Causes
– Gastrointestinal Disorders: Celiac disease, IBD, gastric bypass surgery (malabsorption)
– Rheumatologic Diseases: RA, AS (chronic inflammation and glucocorticoid use)
– Hematologic Disorders: Multiple myeloma, mastocytosis
– Chronic Kidney Disease: Mineral and bone disorders (CKD-MBD)
– Chronic Liver Disease: Impaired vitamin D metabolism
4. Medications
– Glucocorticoids: >5 mg prednisone equivalent daily for >3 months
– Aromatase Inhibitors: Used in breast cancer treatment
– Androgen Deprivation Therapy: For prostate cancer
– PPIs: Long-term use may impair calcium absorption
– Anticonvulsants: Phenytoin, phenobarbital affect vitamin D metabolism
5. Lifestyle Factors
– Physical Inactivity: Lack of weight-bearing exercise reduces mechanical loading
– Smoking: Multiple adverse effects on bone metabolism
– Excessive Alcohol: >3 drinks/day inhibits osteoblast function
– Low Body Weight: BMI <19 kg/m² is a significant risk factor
Risk Factors of Osteoporosis
Risk assessment is critical for identifying individuals who would benefit from screening and preventive interventions:
Non-Modifiable Risk Factors
– Age: Risk doubles every decade after age 50
– Female Sex: Women have lower peak bone mass and experience menopause-related loss
– Race/Ethnicity: Caucasian and Asian populations at higher risk
– Family History: Parental hip fracture increases risk 2-3 fold
– Early Menopause: <45 years natural or surgical
– Previous Fracture: Especially vertebral or hip fracture
Modifiable Risk Factors
– Low Calcium/Vitamin D Intake
– Sedentary Lifestyle
– Current Smoking
– Excessive Alcohol (>3 drinks/day)
– Low Body Weight (BMI <19)
– Frequent Falls: Impaired balance, vision problems, medications
Disease-Specific Risk Factors
– Type 1 Diabetes
– Hyperthyroidism
– Chronic Malabsorption
– Rheumatoid Arthritis
– Chronic Liver Disease
The FRAX tool (Fracture Risk Assessment Tool) developed by WHO incorporates many of these factors to estimate 10-year probability of major osteoporotic fracture.
How Is Osteoporosis Diagnosed?
Osteoporosis is diagnosed through a combination of medical history, physical exams, lab tests, and bone density scans. Here’s a simple breakdown:
1. Medical Checkup
– Health History: Your doctor will ask about past fractures, family history, medications, and lifestyle factors (like diet and exercise).
– Physical Exam: Checks for height loss, spine curvature (kyphosis), or tender spots on the back.
– Lab Tests: Blood and urine tests help rule out other causes of bone loss (e.g., vitamin D deficiency, thyroid issues, or kidney problems).
2. Bone Density Test (DXA Scan)
– What It Does: Measures bone strength, usually at the hip and spine.
– Results Explained:
– Normal: T-score -1.0 or higher
– Osteopenia (Mild Bone Loss): T-score between -1.0 and -2.5
– Osteoporosis: T-score -2.5 or lower
– Severe Osteoporosis: T-score -2.5 or lower with a past fracture
– Who Needs It?
– Women 65+, men 70+
– Younger adults with risk factors (e.g., fractures, steroid use)
– Anyone being monitored for treatment
3. Other Tests (If Needed)
– Spine X-rays/VFA: Detects hidden spine fractures.
– QCT/Peripheral Scans: Alternative tests, but DXA is the gold standard.
Why It Matters
Early diagnosis helps prevent fractures and guides treatment. If you’re at risk, talk to your doctor about getting checked!
Difference Between Osteoporosis and Osteoarthritis
While both conditions commonly affect older adults and involve the musculoskeletal system, they are distinct entities:
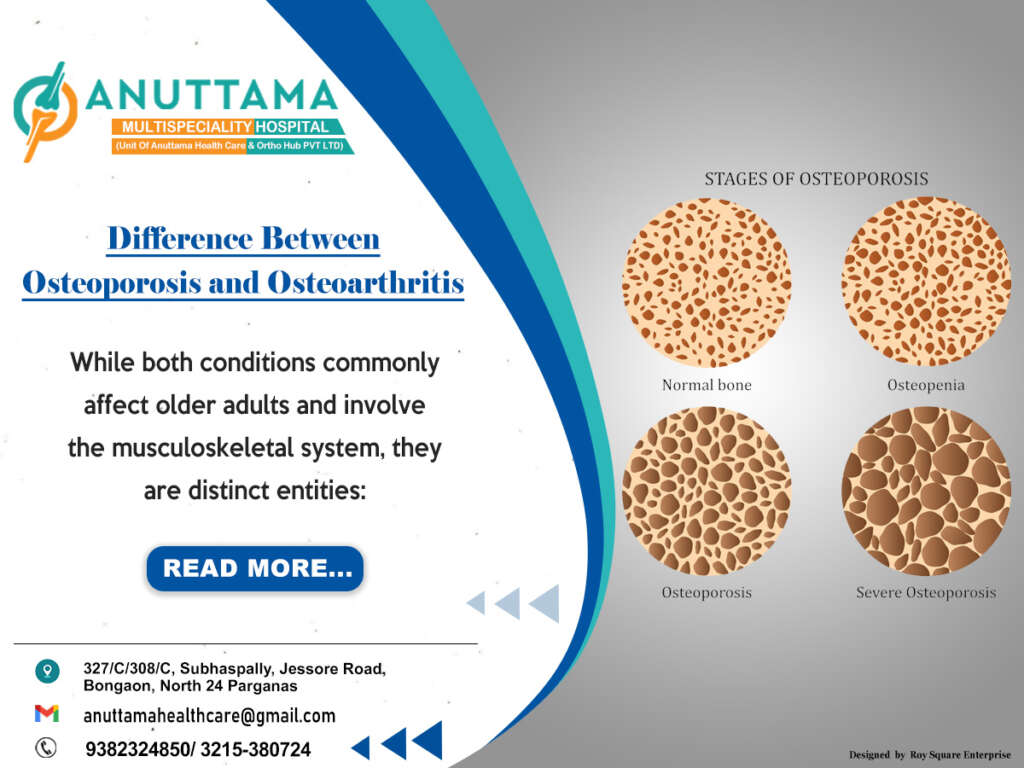
Osteoporosis:
– Primarily a metabolic bone disorder
– Pathologic feature: Reduced bone mass and microarchitectural deterioration
– Main consequence: Increased fracture risk
– Pain typically only with fractures
– Diagnosis by DXA scan
– Treatment focuses on preventing bone loss/resorption
Osteoarthritis:
– Degenerative joint disease
– Pathologic feature: Cartilage breakdown and joint remodeling
– Main consequence: Joint pain and stiffness
– Pain is primary symptom (mechanical pattern)
– Diagnosis by clinical exam and plain radiographs
– Treatment focuses on pain management and joint preservation
Important to note that these conditions frequently coexist, particularly in elderly patients, and may interact – for example, vertebral fractures from osteoporosis can alter spinal mechanics and accelerate degenerative changes.
Osteoporosis Treatment : Building Stronger Bones Safely
Osteoporosis weakens bones silently, but with proper medical guidance and healthy habits, you can protect your bone health effectively. Here’s what you should know about safe and responsible osteoporosis management.
Medical Approaches to Protect Your Bones
– Prescription Therapies:
– Specialized medications exist that either slow bone loss or help rebuild bone strength.
– These treatments require medical supervision and regular monitoring.
– Your doctor will determine the most suitable option based on your bone density and risk factors.
– Hormone-Related Options:
– Some treatments may be considered for postmenopausal women, but these require careful evaluation of benefits versus risks.
Why Self-Medication is Risky
– Osteoporosis medications must be carefully managed by healthcare providers.
– Using it incorrectly may cause side effects or make it less effective.
– Never start, stop, or change treatments without consulting your doctor.
Lifestyle: Your Everyday Bone Protection
Nutrition for Strong Bones
– Calcium-Rich Foods: Dairy, leafy greens, almonds, and fortified products.
– Vitamin D Sources: Sunlight, fatty fish, and egg yolks (supplements may be needed if levels are low).
– Balanced Diet: Include enough protein and minerals for overall bone support.
Exercise Smartly
– Weight-Bearing Activities: Walking, dancing, or stair climbing help maintain bone density.
– Strength Training: Light resistance exercises improve bone and muscle strength.
– Balance & Flexibility: Yoga or tai chi reduces fall risk.
Fall Prevention at Home
– Keep floors clutter-free and well-lit.
– Install grab bars in bathrooms if needed.
– Wear supportive, non-slip footwear.
Monitoring & Long-Term Care
– Regular Bone Density Scans: Help track progress and adjust treatment if necessary.
– Doctor Consultations: Essential to reassess medication needs over time.
Key Message:
- Consult your doctor—they will create a safe, personalized plan.
- Lifestyle matters—good nutrition and exercise support medical treatment.
- Never self-prescribe—osteoporosis medications require professional oversight.
Prevention of Osteoporosis
Maintaining bone health is important throughout your life:
Childhood/Adolescence
– Maximize peak bone mass through:
– Adequate calcium/vitamin D intake
– Regular physical activity
– Avoidance of smoking/alcohol
Adulthood
– Maintain healthy lifestyle habits
– Regular weight-bearing exercise
– Avoid excessive dieting/weight fluctuations
Postmenopausal Women/Older Adults
– Ensure adequate calcium/vitamin D
– Regular bone density screening when indicated
– Timely initiation of pharmacotherapy when appropriate
Special Cases
– Glucocorticoid Users: Start bone protection therapy if anticipated use >3 months
– Transplant Patients: High fracture risk; early intervention needed
– Cancer Patients: Address bone health in treatment planning
10 Key FAQs About Osteoporosis – Clear & Concise Answers
1. Can osteoporosis be cured?
While not fully reversible, treatments can strengthen bones and prevent fractures, helping patients stay active.
2. When should bone density tests start?
Women at 65, men at 70—but earlier (from age 50) for high-risk individuals (fractures, steroids, family history).
3. Are osteoporosis medications safe long-term?
Yes, when monitored. Bisphosphonates are often used for 3-5 years, while biologics like denosumab need regular check-ups.
4. Do men get osteoporosis?
Yes! 1 in 4 osteoporotic fractures occur in men, yet it’s often overlooked.
5. What’s the best exercise for bones?
Mix weight-bearing (walking, dancing), strength training, and balance exercises—adjust based on ability.
6. How does menopause impact bones?
Estrogen drop speeds bone loss—up to 20% in 5-7 years. Early action is key.
7. Are bone density tests risky?
No! DXA scans are painless, quick, and use very low radiation (less than a chest X-ray).
8. Can osteoporosis affect dental health?
Yes, jawbone loss may complicate dental work. Tell your dentist if you have osteoporosis.
9. How often should bone density be checked?
Typically every 1-2 years, or more often if treatment adjustments are needed.
10. What’s new in osteoporosis treatment?
Emerging options like romosozumab (dual-action drug) and advanced anabolic therapies show promise.